Introduction
When it comes to billing and coding medical claims, accuracy is not just important, it’s paramount. Ensuring your physical therapy medical claims are error-free not only helps you get reimbursed faster for the full amount you deserve, but also plays a crucial role in preventing abuse and ensuring patients receive the care they need. Among the strict regulations set by Medicare is the 8 minute rule for physical therapy, a rule that demands your attention and diligence.
The 8-minute rule is not just a regulation, but a crucial factor in ensuring accurate billing for physical therapy services. This blog delves into the nuances of the 8 minute rule billing, equipping you with the knowledge you need for precise billing.
What is the 8 Minutes Rule?
Before we delve into the specifics, let’s start with a brief overview of the 8-minute rule in Medicare. This rule, which isn’t always straightforward, plays a significant role in physical therapy billing services. Now, let’s get into the definition and details…
According to the CMS (Medicare and Medicaid), there are 15 billable units.
“For any single timed CPT code in the same day measured in 15-minute units, providers bill a single 15-minute unit for treatment greater than or equal to 8 minutes.”
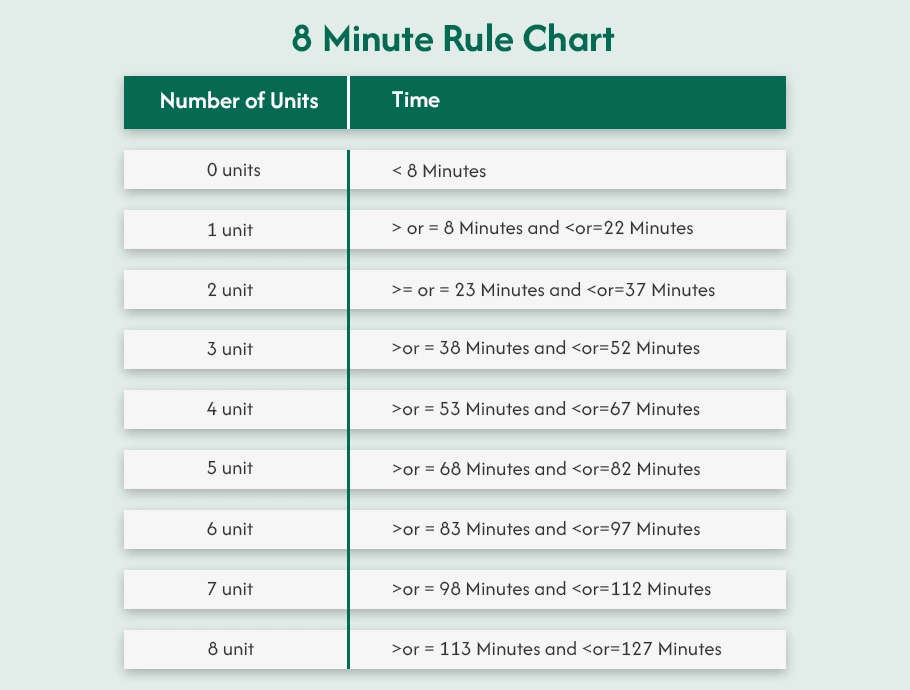
At its core, the 8-minute rule is a method for determining the number of ‘billable units’ that can be charged in rehabilitation. These units, which are based on 15-minute increments, are billed once the initial 8 therapy minutes of treatment have been met.
Here’s a quick overview of the 8 minute rule chart.
Timed and Untimed Therapy Codes
It’s crucial to reiterate the importance of distinguishing between timed and untimed CPT codes.
Timed Codes
These codes represent services directly provided by the therapist, such as manual therapy, therapeutic exercise, and neuromuscular re-education. The 8-minute rule, which stipulates that a service must be provided for a minimum of 8 minutes to be billed, applies to these CPT codes.
Untimed Codes
These codes encompass a wide range of services that don’t require direct, one-on-one contact, such as hot packs, electrical stimulation, and paraffin wax baths. The 8 minute therapy rule doesn’t apply to them.
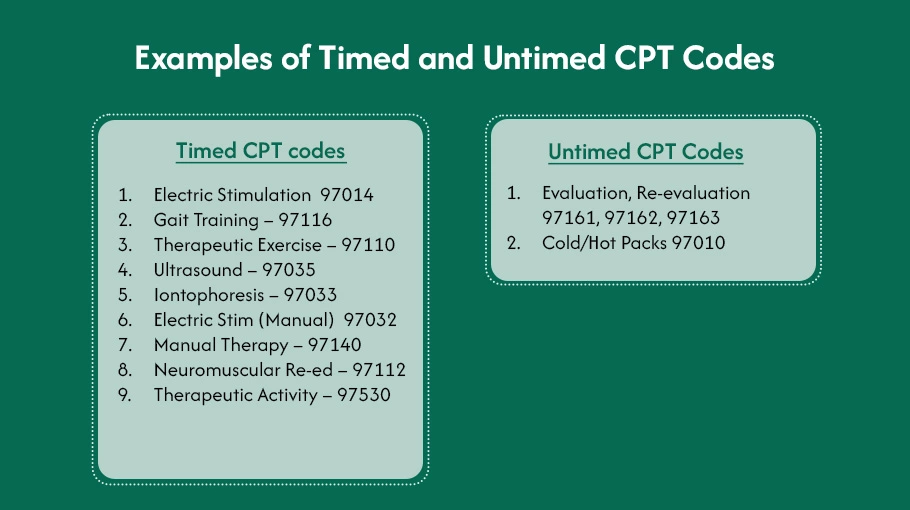
Examples of Timed and Untimed CPT Codes
Timed CPT codes
- Electric Stimulation 97014
- Therapeutic Exercise – 97110
- Ultrasound – 97035
- Iontophoresis – 97033
- Electric Stim (Manual) 97032
- Manual Therapy – 97140
- Neuromuscular Re-ed – 97112
- Therapeutic Activity – 97530
- Gait Training – 97116
Untimed CPT Codes
- Evaluation, Re-evaluation 97161, 97162, 97163
- Cold/Hot Packs 97010
Difference Between “8 Minute Rule” Vs. “Rule of Eights”(AMA)?
Despite their seemingly similar names, understanding the nuances of the 8-minute Rule and the Rule of eights is more than just a theoretical exercise. It’s a crucial step towards ensuring accurate billing and coding practices in your daily healthcare operations.
Rule of 8s
The Rule of eights, a key component of the American Medical Association’s (AMA) guidelines, is not to be taken lightly. It focuses on individual units within a service, stipulating that each unit of a time-based service must involve at least eight minutes of direct contact. This knowledge can significantly impact your billing and coding practices, making it a crucial aspect of your professional toolkit.
The Rule of 8s is applied to each timed service separately.
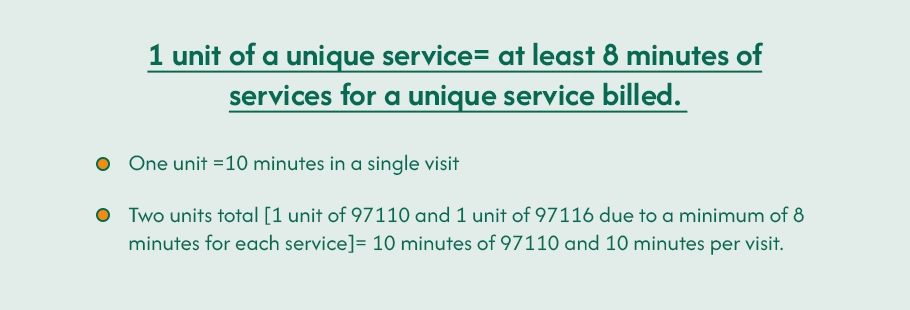
1 unit of a unique service= at least 8 minutes of services for a unique service billed.
- One unit =10 minutes in a single visit
- Two units total [ 1 unit of 97110 and 1 unit of 97116 due to a minimum of 8 minutes for each service]= 10 minutes of 97110 and 10 minutes per visit.
8 Minute Rule
For Medicare, the 8-minute Rule is specific and significant. It looks at the total time spent with the patient across all timed codes for a session. Being aware of this Rule can help you ensure accurate billing and coding for Medicare patients. Not adhering to this Rule could result in incorrect billing, leading to potential financial loss for your practice.
The Medicare 8 minute rule considers total minutes and units for timed codes.
- One unit = at least 8 minutes of service are needed.
- Two units = at least 23 minutes of service are needed.

The Rule is consistently implemented whether it’s two pt units of the same services (97110) or 1 unit of two different services (97110 and 97116).
How to Calculate Billable Units?
Calculating Billable Units
After getting insight into the 8-minute rule of physical therapy, you need to understand how to calculate your billable units. Whether you have an in-house team or outsource your physical therapy billing and coding services, you must know the complete process.
Outsource Physical Therapy billing coding and billing services to boost your revenue by up to 25%.
Here’s how to calculate pt billing units under the 8-minute rule:
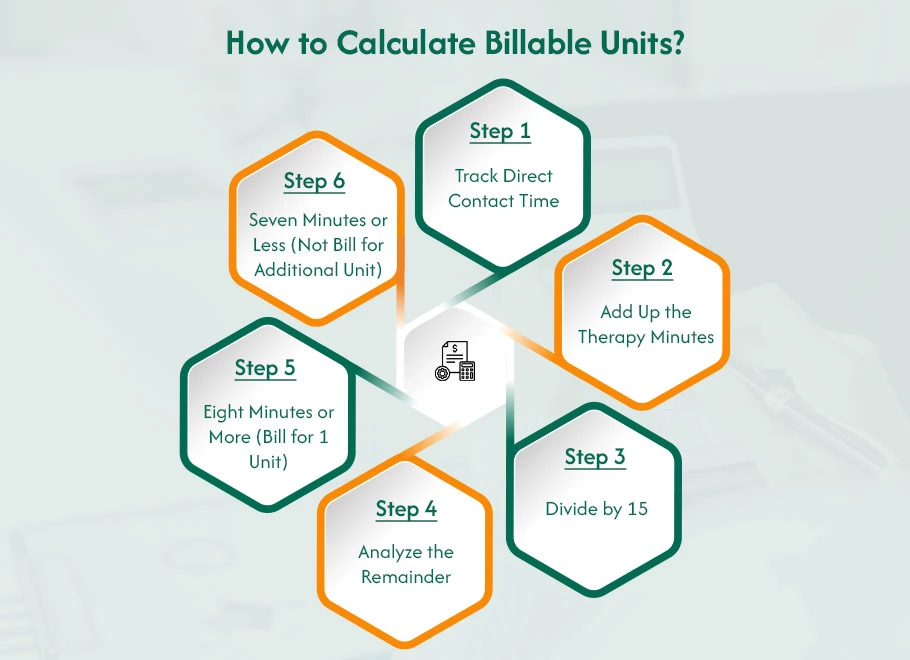
- Using timed CPT codes, document the total minutes of direct, one-on-one therapy provided during the session.
- Combine the documented minutes for all timed services.
- Divide the total accumulated minutes by 15 (the standard billing unit increment).
- Look at the remaining minutes after the division.
- If eight minutes or more remain, you can bill for one additional unit.
- If seven minutes or less remain, you cannot bill for an additional unit.
Example
A physical therapist spends 28 minutes with a patient, providing 15 minutes of therapeutic exercise (timed code) and 13 minutes of manual therapy (timed code).
Total Time = 15 minutes + 13 minutes = 28 minutes
Units = 28 minutes / 15 minutes/unit = 1 unit with a remainder of 13 minutes
Since the remainder (13 minutes) is more than eight minutes, you can bill for one additional unit (total of 2 units).
Mixed Remainders
Addressing Mixed Remainders When Multiple Services are Involved
Complex scenarios may arise when using multiple timed codes within a session. However, if the sum of the remaining minutes from each timed service after the 15-minute division is eight minutes or more, you can confidently bill for an additional unit, even if the individual remainders are less than eight minutes on their own.
For instance, imagine providing 7 minutes of manual therapy and 5 minutes of therapeutic exercise, with a total time of 22 minutes.
- Individual remainders
Manual therapy (0 minutes), Therapeutic exercise (2 minutes)
- Combined remainder
0 minutes + 2 minutes = 2 minutes
However, since Medicare considers the “cumulative” effect of these remainders, you can still bill for one unit because the total remaining time (2 minutes) is greater than the 8-minute threshold.
Another Example:
| Code | Description | Minutes | Units | Remainder | New Units |
| 97110 | Therapeutic | 18 | 1 | 3 | 1 |
| 97140 | Manual | 20 | 1 | 5 | 2 |
| Total | 38 | 2 | 8 | Total Units=3 | |
If you have a total of 38 minutes, this equals three units. To determine which service requires an additional unit, divide 38 by 15. Each code is assigned as one unit. The second unit is billed for the remaining 8 minutes until manual therapy covers more of the remaining time. This practical application of the guidelines can help you ensure accurate billing for multiple-timed services.
Rest assured to us for physical therapy billing, coding and Revenue Cycle analysis, you can schedule a demo now to experience error-free billing and gain a deeper understanding of the process.
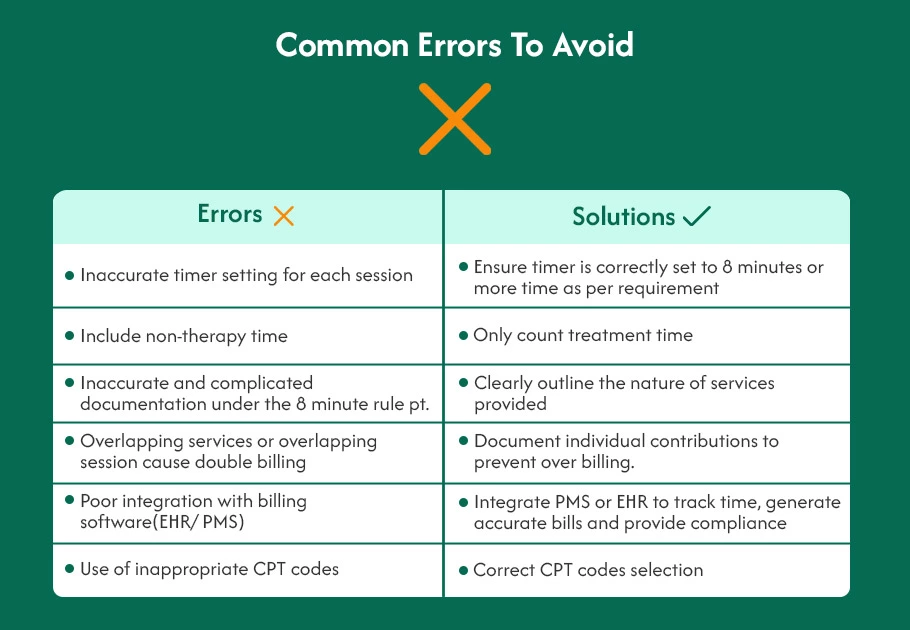
How to Avoid Problems with the 8 Minute Billing Rule ?
You can use the 8-minute therapy rule to avoid coding errors that cut down the denial rate. Here are some common mistakes you must avoid while applying this rule.
Where Does Physical Therapy Billings Steps In?
The 8-minute rule states that Medicare will only reimburse for outpatient physical therapy services if the documented time spent on therapeutic activities reaches or exceeds 8 minutes per session. This seemingly straightforward rule can be tricky to implement. Activities like patient education, gait training, and manual therapy must be meticulously documented to meet the 8-minute threshold. Failure to meet this rule can result in denied claims and financial loss for your practice.
Here’s how our dedicated team specializing in physical therapy can help you understand the 8-minute rule maze:
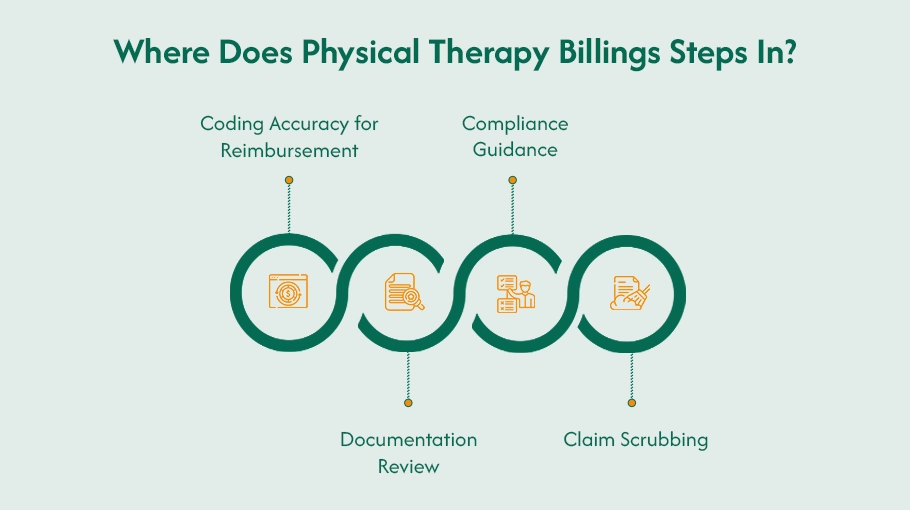
Coding Accuracy for Reimbursement
Understanding the Nuances
Our physical therapy billing company experienced coders are well-versed in the specific Current Procedural Terminology (CPT) codes used for physical therapy services. We have a deep understanding of the intricacies of the 8-minute rule and how it applies to different treatment modalities, such as manual therapy (97110, 97140), therapeutic exercise (97110), electrical stimulation (97035), and gait training (97112). For example, if you spend 12 minutes on manual therapy and 10 minutes on therapeutic exercise, we’ll code for one unit of 97140 (manual therapy) and one unit of 97110 (therapeutic exercise), reflecting the time you dedicated to each activity.
Time-Based Coding Expertise
We can accurately translate the time spent on each therapeutic activity into the appropriate CPT codes. This ensures Medicare recognizes the total value of the services you provide. For instance, if you spend 12 minutes on manual therapy and 10 minutes on therapeutic exercise, we’ll code for one unit of 97140 (manual therapy) and one unit of 97110 (therapeutic exercise), reflecting the time you dedicated to each activity. This expertise in time-based coding can help ensure that you are reimbursed accurately for the services you provide.
Staying Up-to-Date on Coding Changes
Physical therapy coding is constantly evolving. Our staff proactively stays current with any changes or clarifications related to time-based coding and the 8-minute rule. We ensure your coding practices remain compliant by informing you about updates from the American Medical Association (AMA) and the Centers for Medicare & Medicaid Services (CMS).
Documentation Review
Detailed Scrutiny
Our billing team needs to do more than skim your notes. They meticulously review your documentation for each session, ensuring it reflects the following crucial details:
Start and End Times
Each therapeutic activity’s specific start and end times must be documented in your notes. For example, “Manual therapy: 10:25AM – 10:37 AM” or “Therapeutic exercise: 10:00 AM – 10:18 AM.”
Specific Treatment Provided
The type of treatment provided (e.g., manual therapy, therapeutic exercise, electrical stimulation) must be identified. This helps with accurate CPT code selection.
Duration of Each Activity (Minutes)
The duration of each activity must be documented in minutes. This is crucial for meeting the 8-minute rule threshold. If documentation needs to be clarified or added time entries, our staff will consult you to ensure accurate documentation.
If there are any inconsistencies between your documentation and the CPT codes used, we’ll work with you to bridge the gap and ensure your claims accurately reflect the services delivered. For instance, if your notes show 10 minutes of manual therapy but the code used only accounts for 8 minutes, we will help you revise your documentation or adjust the code selection to represent the time spent accurately.
Compliance Guidance
Regulatory Expertise
We stay on top of all Medicare regulations, including the latest interpretations and updates to the 8-minute rule. They proactively inform you of any changes that might impact your billing practices. This could include updates on acceptable documentation practices, changes in specific CPT code interpretations, or clarifications on handling situations where treatment sessions fall below the 8-minute threshold.
Staying Ahead of the Curve
We anticipate potential compliance issues related to the 8-minute rule and guide best practices to ensure your documentation and coding always meet Medicare’s requirements. For example, we suggest using time trackers or standardized note templates to ensure consistent documentation of treatment times. This expertise in compliance guidance can help you avoid potential issues with the 8-minute rule and ensure that your billing practices are always in line with Medicare’s requirements.
Advanced Software for Accuracy
We utilize sophisticated software to scrub your claims before submission. This software scans for potential errors in coding or documentation related to the 8-minute rule. These errors could include missing time entries, inconsistencies between time documented and code used, or unclear descriptions of treatment activities. By identifying these issues before submission, we can ensure that your claims are accurate and compliant with Medicare’s requirements.
Identifying Red Flags
The software can flag potential red flags that could trigger denials from Medicare, such as missing time entries, time inconsistencies, or unclear descriptions of treatment activities. By identifying these issues before submission, we can help you avoid claim denials and ensure that your claims accurately reflect the services delivered.
Missing time entries
If a treatment session lacks documented start and end times for specific activities, the software will flag it for review.
Time inconsistencies
If the total documented time for all activities doesn’t reach 8 minutes, the software will flag it, prompting us to investigate and potentially adjust the codes or documentation.
Unclear descriptions
If descriptions of treatment activities are ambiguous, the software may flag it for clarification to ensure accurate coding.
The benefits of our company extend beyond just the 8-minute rule. We can handle the entire billing cycle, from coding accuracy to claim submission and review. This comprehensive approach frees up your valuable time to focus on what matters most – your patients.
Don’t let the 8-minute rule steal your time and revenue. Schedule a free consultation with our physical therapy billing experts today!